A new meta-analysis, which brings together a significant amount of research on SARS-CoV-2 and related coronavirus protection, provides the best available evidence for physical distancing, mask use, and eye protection.
In the absence of a vaccine or other treatments that would slow the spread of the virus, public health organizations have recommended a series of social and behavioral changes to reduce the transmission.
In addition to frequent handwashing, authorities have emphasized the importance of physical distancing: leaving the house less frequently and maintaining as much distance as possible from others at all times while outside.
They also recommend the use of face masks and eye protection, particularly among healthcare workers and people working in the community.
However, experts are still debating when and how these policies should be implemented — including what constitutes the minimum distance that people should maintain from one another, when and where to wear personal protective equipment, and how effective this equipment is against the virus.
To address this, the World Health Organization (WHO) commissioned the present meta-analysis, which was conducted by an international team of researchers, clinicians, patients, and policy experts.
The authors sifted through over 20,000 research papers to find 44 comparative studies that related to the protective benefits of physical distancing, wearing face masks, and wearing eye protection.
The included studies addressed infection with the SARS-CoV-2 virus, the SARS virus, which caused an outbreak in the early 2000s, or the MERS-CoV virus, which caused an outbreak in the early 2010s. Because SARS-CoV and MERS-CoV are similar to SARS-CoV-2, research into these pathogens can provide insight.
The authors found no differences in the effectiveness of distancing, face masks, and eye protection in responses to the three coronaviruses and, therefore, feel confident in pooling the findings from the various studies.
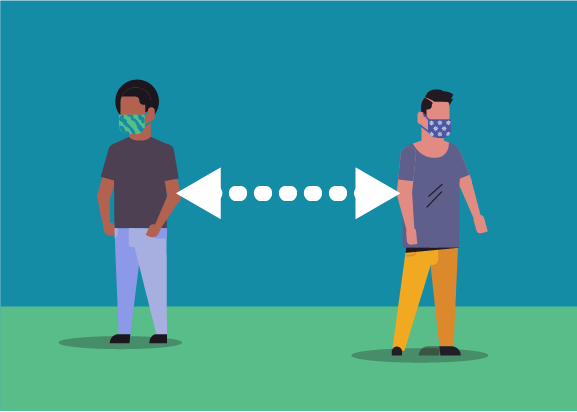
The authors conclude that there is good evidence that maintaining a minimum distance of 1 meter, or about 3.3 feet, from other people is likely to have a significant effect on reducing the spread of the virus.
Across 38 studies that included information about distancing, infection rates overall were reduced to 2.6% when maintaining a distance of more than 1 meter from a person with the infection. By comparison, among studies in which distancing was less than 1 meter, the infection rate was 12.8%.
Furthermore, the authors found evidence that increasing the distance to 2 meters was likely to have an even greater effect.
Dr. Derek Chu, a lead author of the study,
said: “We found that with each additional 1 meter of distance, the relative degree of protection increased about two-fold. […] Overall, [this] supports measures of at least 2 meters when feasible and possible.”
The authors point out that their finding of increased risk of infection at 2 meters has implications for the cut-off for contact tracing, and they suggest that 2 meters should be adopted universally.
The authors note that there is a consensus that the virus is transmitted through water droplets expelled from a person’s throat or nose when they cough or sneeze. These droplets are unable to stay airborne for very long, which is likely to explain why distances of at least 1 meter significantly reduce transmission.
Evidence of whether the virus can also transmit as an aerosol — surviving on very small particles that are also expelled as a person coughs and sneezes — has been mixed. These particles may be able to stay airborne for longer and thus infect a person at a greater distance.
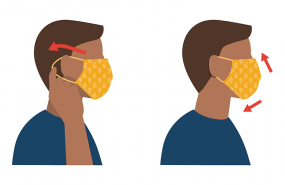
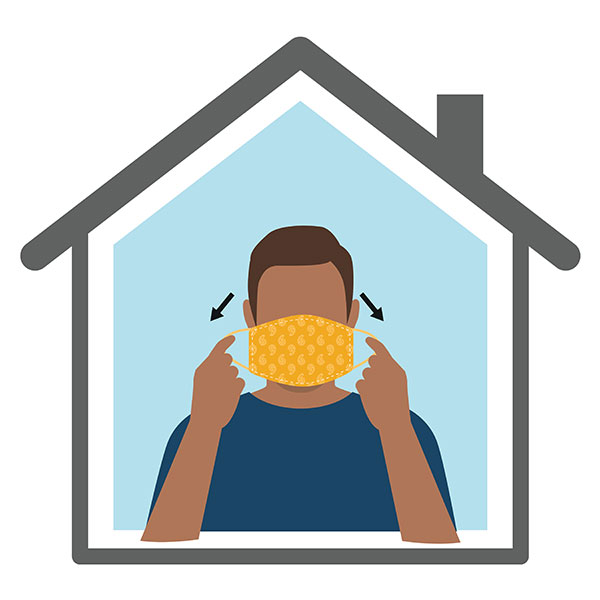
As well as maintaining a minimum distance, face and eye masks are also designed to stop the spread of the virus, either by reducing the amount that a person expels or reducing the amount that can access a person’s mouth or eyes and, therefore, their respiratory system.
The authors found good evidence that both face masks and eye masks significantly reduced transmission of the virus for health care workers and people working in the community, such as care home workers.
The odds of developing an infection with a coronavirus were reduced by 78% when wearing any mask, compared with the odds of infection when not wearing a mask. When using masks that conform to the
N95 standard, this figure increased to 96%.
According to co-lead study author Dr. Holger Schünemann, who, like Dr. Chu, works at McMaster University, in Ontario, Canada, “Although the direct evidence is limited, the use of masks in the community provides protection, and possibly N95 or similar respirators worn by healthcare workers suggest greater protection than other face masks.”
In a
Lancet podcast, Dr. Schünemann confirmed that even wearing a “self-made face mask is better than having no face mask.”
While the study presents the best available evidence for policymakers to draw on when making key decisions about how to respond to the pandemic, particularly as lockdown measures begin to ease, the authors acknowledged their analysis has some limits.
None of the currently available studies looking at the protection afforded by physical distancing, face masks, and eye protection were randomized, and many of the studies did not specify exact distances.
Around three-quarters of the studies focused on healthcare settings, which means that while the evidence to support wearing face masks in these contexts is good, there is more uncertainty surrounding the use in nonhealthcare settings.
However, the authors state that once they had taken account of low levels of use of the highly effective N95 respirator masks in the community, they found other types of masks to be equally effective in both hospital and community settings.
Nonetheless, in the absence of randomized controlled trials that can provide more information and a greater degree of certainty — and until a vaccine or effective treatment is developed — the research presents policymakers and clinicians with valuable interim information on which to base key decisions.
MedicalNews Today